"Recently Approved 'Living Drug' Offers Hope for Saving More Cancer Patients"
Toni English’s medical team was giddy.
It was six weeks after English had completed an experimental cancer treatment, and she had arrived at the Orlando Health Cancer Institute in Florida with her husband to see the results of her latest scan.
Her team gathered in a patient exam room on the second floor of the institute. English could sense the excitement. Someone held up a phone, ready to take English’s picture. Her oncologist stood near a computer screen and pointed to an image. “Here’s the picture of your lungs before treatment,” he said. In English’s left lung, the bulbous white splotch of a tumor was clearly visible — about the size of a nectarine. Then the oncologist showed English her most recent scan. That white spot was gone. “It was history,” English says. The team waited for a reaction. English stayed silent for a moment and then said, “Well, good! Isn’t that what we were expecting?”
English, who is in her 60s, had mucosal melanoma, a rare form of the disease — and it can be deadly. Five years after receiving a diagnosis, only about a quarter of patients are still alive. English’s melanoma had become metastatic, creeping beyond its initial home in her nose to her lungs, kidney, and brain.
Existing therapies can shrink these kinds of tumors and keep the cancer under control, but they don’t help every patient. Over the last three years, English had been trying a nightmarish carousel of treatments including surgery, radiation, and drugs that boost the immune system. Looking back on that time, “it was pretty rough,” she says, but “I was just doing what I had to do.” Still, the cancer persisted, and English thought she was out of options — until her doctor told her about a clinical trial for the new drug.
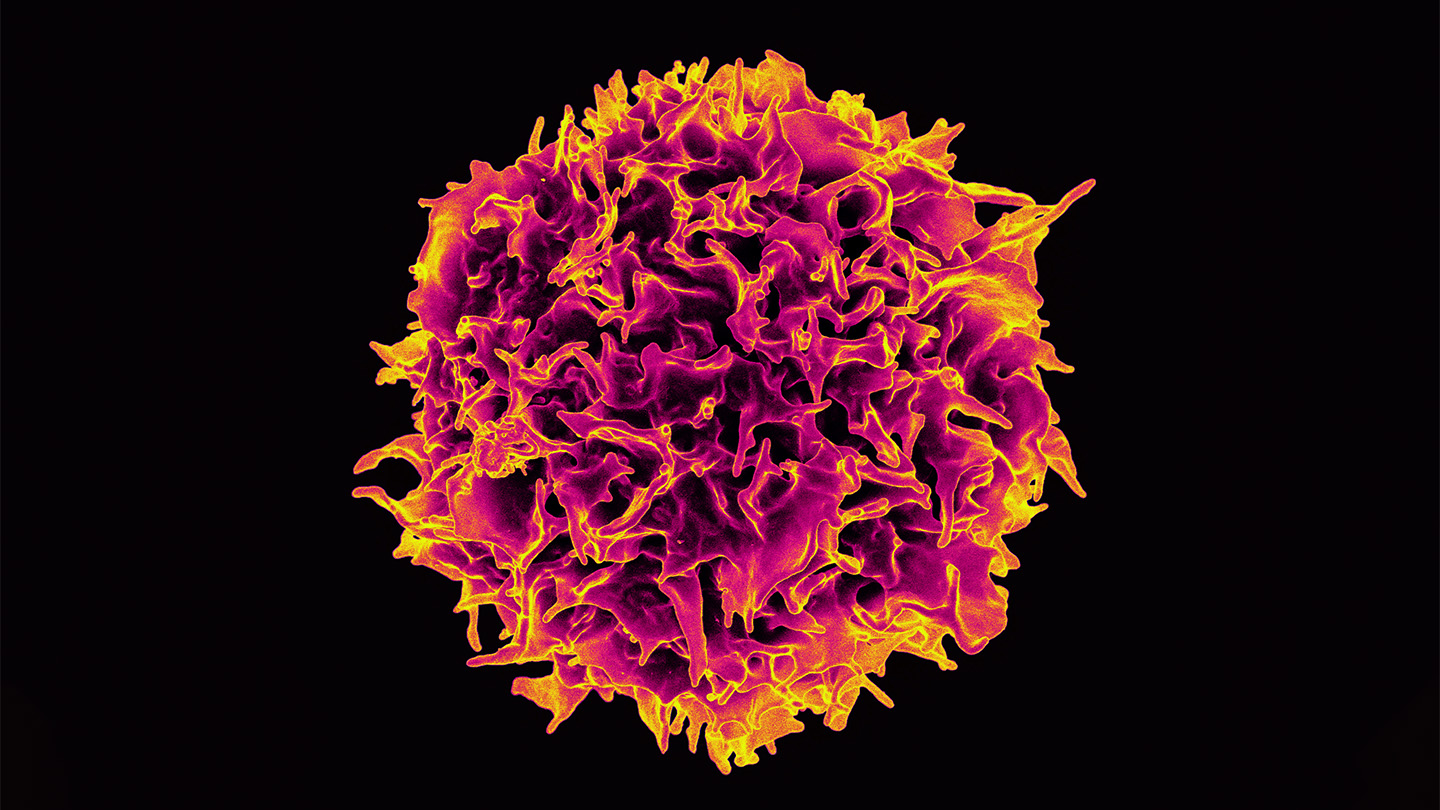
The trial was testing a treatment developed by the company Iovance Biotherapeutics, and it was unlike anything English had tried: a “living drug” made up of immune cells called T cells. Tumor-infiltrating lymphocyte therapy, or TIL therapy, takes cancer-targeting T cells from a patient’s tumor, grows them to the billions in the lab, and then infuses them back into the body. This massive influx zeroes in on and attacks cancer cells and, in some cases, appears to wipe out every last one.
Now, six years after English saw her promising scan, TILs are available for patients beyond clinical trials or early access programs. In February, the U.S. Food and Drug Administration approved Iovance’s TIL therapy, called lifileucel, brand name Amtagvi, for advanced melanoma. Though other T cell–based therapies that engineer patients’ cells have been approved for blood cancers, this is the first time the FDA has approved a T cell therapy for a solid tumor. Such tumors make up some 90 percent of new cancer cases worldwide and may kill more than 550,000 people in the United States this year.
Amtagvi didn’t work for everyone with advanced melanoma — not by a long shot. English was one of the lucky ones. The FDA based its approval on 73 people, including English, who were part of a larger clinical trial. Of those 73, just three saw their cancer disappear. But nearly a third of the patients saw some benefit. Though the number may sound low, TIL therapy can be a lifesaver for some people. And as scientists get a better handle on which patients will benefit and which T cells are most powerful, outcomes should only improve, says cancer surgeon Udai Kammula of the University of Pittsburgh.
The drug’s approval has cracked the door open to a potential wide world of TIL therapies, Kammula says. Dozens of TIL trials around the world, including three from Kammula’s team, are testing treatment variations and more types of cancer, including breast, pancreatic, and colorectal cancers, some of the deadliest forms of the disease.
Oncologist Steven Rosenberg, chief of the Surgery Branch of the National Cancer Institute in Bethesda, Md., pioneered the technology. He began treating patients with TILs in the late 1980s. Rosenberg has now seen dozens of people survive more than a decade cancer-free. “That’s pretty convincing evidence that cure is possible,” he says.
Scientists today know that our immune systems can attack cancer, but when Rosenberg started working at the National Cancer Institute in 1974, the idea was dogged with doubts. Most scientists just didn’t think our immune systems could tell the difference between a healthy cell and a cancerous one.
Rosenberg wasn’t so sure. In 1968, he saw a patient who had undergone surgery more than a decade earlier to remove most of his cancer-ridden stomach. Tumors also riddled his liver and lymph nodes, but his doctors couldn’t operate on them, and he hadn’t received any further treatment.
While operating on the patient during an unrelated gallbladder surgery, Rosenberg noticed that the man’s cancer had entirely disappeared. Somehow, he had fully recovered from cancer without additional treatment. “One of the rarest events in medicine,” Rosenberg wrote in a 2021 editorial that chronicled the history of cancer immunotherapies.
That remarkable recovery stuck in his mind. The man’s immune system had probably hunted down and destroyed the cancer, Rosenberg thought. The case helped put him on a path toward understanding the immune system’s cancer-fighting powers. And “what better place to look for cells doing battle against cancer than within the cancer itself?” he says.
Scientists now know that a variety of factors can suppress T cells’ natural tumor-fighting abilities. So our immune systems sometimes need help to quash cancer.
In 1988, after years of experiments in the lab and the clinic, Rosenberg’s team reported a breakthrough. In a trial of 20 people with melanoma that had spread from the skin to other places in the body, tumors shrank in more than half of participants treated. The patients had received TILs, cells surgically removed from their tumors and expanded to large numbers in the lab, along with infusions of interleukin-2, or IL-2, a molecule that helps the cells grow. The work “demonstrated for the first time that lymphocytes could be used as a living drug for treating cancer,” Rosenberg says.
His team’s results inspired a decades-long effort to improve TIL therapy. It’s an idea that was ahead of its time, says Jae Park, a hematologist-oncologist at Memorial Sloan Kettering Cancer Center in New York City. And while researchers were getting TIL off the ground, Rosenberg’s team and others were also working on other ways to harness T cells to fight cancer.
In TIL therapy, doctors remove part of a patient’s tumor (Step 1) and extract tumor-infiltrating lymphocytes, a type of T cell (2). Scientists grow billions of them in the lab with interleukin-2, a molecule that boosts cell growth (3). The patient undergoes chemotherapy to prepare the body to accept the infusion of T cells, which are injected into the bloodstream (4).
One method that took off faster than TIL therapy is called CAR T-cell therapy, for chimeric antigen receptor T cells. Using genetic engineering, scientists modify a patient’s own T cells so they can recognize a specific cancer cell signal. These customized cells can hunt down certain cancers like a pack of hounds with the scent of prey in their noses. Since 2017, the FDA has approved a half dozen CAR T-cell therapies for certain leukemias, lymphomas and multiple myeloma, which develops inside the bone marrow (SN: 6/27/18).
But trying to engineer designer T cells that recognize and lock onto cells from solid tumors has been a thorny challenge. It’s tricky to find a unique molecular signal on the tumor cells that clearly shouts “cancer” to the T cells. So far, the therapy has been approved only for liquid cancers, like those of the blood.
“Efforts to use CAR T-cells in solid tumors have been uniformly unsuccessful,” Kammula says.
CAR T-cell therapy probably wouldn’t have worked for English’s melanoma, or any disease like hers. But that’s where TIL can come in.
“TIL therapy is a relatively primitive treatment,” says Marco Donia, an oncologist at the University of Copenhagen Herlev Hospital and Gentofte Hospital in Denmark. The therapy approved by the FDA doesn’t rely on genetic engineering nor a predefined molecular target. It’s just a messy mix of T cells grown from a patient’s tumor.
In fact, as CAR T-cells and a related therapy called T-cell receptor therapy emerged, “people started to think that TIL would be obsolete,” says Sylvia Lee, an oncologist at Fred Hutchinson Cancer Center in Seattle. “It was not as sophisticated or as elegant as these fancier ways to create designer T cells.”
Scientists simply surgically remove part of a patient’s tumor, grow vast quantities of T cells from the tumor over about a month, and then infuse the cells back into the patient’s bloodstream. TILs have an innate tumor-detecting ability and can kill cancer cells, sometimes eliminating the disease. But how exactly everything works — and why it sometimes doesn’t — is something scientists don’t completely understand, Lee says.
One aspect of TIL biology seems clear: Tumor-infiltrating cells have a sort of sixth sense for the mutated proteins that can twist a healthy cell’s fate toward cancer. Some of these mutated proteins, unleashed by simple tweaks to a cell’s DNA, fail to keep cell growth in check; others get growth galloping like a horse touched by spurs.
“The very mutations that cause the cancer are likely to be the Achilles’ heel for treatment,” Rosenberg says. That’s especially relevant for cancers loaded with mutations, like melanomas that form in the skin.
If you rank cancers by mutation level, these melanomas, called cutaneous melanoma, tend to top the list. Not far behind are lung cancer and bladder cancer, which make them promising targets for TIL, says Michael Poch, a urologic oncologist at Moffitt Cancer Center in Tampa, Fla. He’s currently recruiting participants for a TIL clinical trial in people with bladder cancer.
It’s still early days. His team will first test the treatment’s safety in about a dozen patients. But, like many other clinical trials under way, it’s taking TIL in new directions — in this case, with a different type of cancer.
Some cancers carry more genetic mutations, called the tumor mutational burden, than other cancers, though this can vary from person to person. Skin cutaneous melanomas, for example, tend to have far more mutations than uveal melanomas, which affect the eye.
Here, dots represent patient samples and red lines represent the median number of mutations. Having many mutations may make a cancer more susceptible to TIL therapy.
Kammula is steering into territory that’s even less familiar. Rather than tackle another cancer chock-full of mutations, Kammula did an about-face. He’s trying TIL therapy on uveal melanomas. Unlike skin melanomas, these cancers arise in the eye. But they neither carry many mutations nor teem with T cells.
By testing uveal melanoma samples in the lab, Kammula’s team could identify which ones likely contain cancer-fighting T cells. That let the researchers predict how well people will respond to TIL, they reported in April in Nature Communications. It’s an approach that could give doctors a better idea of who might benefit most from treatment and is being tested in a clinical trial expected to be completed in 2027.
Kammula thinks what his team learns from uveal melanoma could serve as a blueprint for treating other cancers. But he notes that improvements in TIL therapy could take many forms — including how best to create an environment in the body where the cancer-fighting cells can thrive.
Amtagvi and most other TIL therapies in the works require knocking down a patient’s immune system before giving them the expanded batch of T cells. “If you’re going to reboot and redevelop the immune system,” he says, “you’ve got to get rid of the old one.”
That takes chemotherapy; later, patients receive a drug to soup up their newly infused TIL. Honing this process could one day make TIL therapy easier for patients, Kammula says. Right now, it’s no cakewalk. “There’s a risk of infection, there’s a risk of death,” he says. “It’s a tough treatment.” And it’s what English went through in her clinical trial in Orlando.
English’s cancer began as a sinus infection. At least, that’s what she thought. It was spring 2015, and her nose felt irritated and dried out, perhaps bothered by pollen. Then came the nosebleeds.
It was no big deal at first, says English, an indefatigable optimist with a soft Southern accent. But the nosebleeds began coming more frequently, and they got more severe. She could actually see that something was growing out of her nostril. It was large, it was black and it was cancer.
The tumor stretched up into her nose, pressed against her right eyeball and filled her sinuses, like an invasive fungus flexing its fingers throughout her face. A surgeon operated and removed everything but a tiny spot near her tear duct. English has since learned that people with tumor masses as large as hers often have to have part of their face cut away. But her surgeon promised he wouldn’t take her eye. Later, radiation zapped the remaining spot, and scans three months, six months and nine months afterward looked good. English seemed to be in the clear.
Then came her 12-month scans. Almost a year to the day after she had completed radiation, the cancer came back. This time, doctors found spots on her lungs, right kidney and brain. English couldn’t believe it. “It was just everywhere,” she says.
Doctors got her started on immunotherapy with drugs called checkpoint inhibitors, which rev up the immune system’s cancer-fighting abilities (SN: 6/25/15). “These medications are great,” Lee says. “They’ve transformed the care of melanoma over the past 10 years.”
But about half of melanoma patients relapse after treatment or don’t respond at all, she says. The drugs didn’t work for English. A different kind of therapy, called gamma knife radiosurgery, had destroyed the tumors in her brain, but even after two kinds of immunotherapy, scans showed cancer still simmering in her kidney and lungs. She asked her oncologist, “What are we going to do now?”
The drug lifileucel, sold as Amtagvi, has been approved for use against melanoma. But it shows promise against other solid tumors too. In a small clinical trial of 28 patients with non-small cell lung cancer, six participants, or 21 percent, saw their tumors shrink after taking the drug. These CT scans show the drug’s effectiveness against one man’s tumors (shown from two angles).
For English and other trial participants, tumor-infiltrating lymphocytes were a last-ditch treatment. English received her TILs on April 2, 2018, a date that stands out in her mind, though the treatment was largely uneventful. She remembers a nurse hanging up the IV bag that delivered more than 7 billion cells into her veins. After the TILs had infused into her body, nurses wheeled English’s bed to the hospital’s intensive care unit for the next step. That’s when things got difficult. Every eight to 12 hours for about two days, English received a high dose of IL-2, which ramps up TIL growth.
It’s a crucial part of the process, but rife with side effects. The medication can cause high fevers, chills, dangerously low blood pressure, kidney problems and fluid to leak from the blood vessels, among other issues.
English doesn’t recall much from that time in the hospital. The treatment left her feeling weak, and sleeping at night was difficult. In the shower, her hair fell out by the handful. But about four days later, English’s strength had built up enough that she could walk laps in the hospital’s halls. She was healthy enough to discharge. Six weeks later, at English’s follow-up visit, she saw the scans showing that her lung tumor had vanished. And six months after TIL therapy, all traces of cancer were gone.
Those drastic results weren’t the norm. Of the 73 participants whose data the FDA considered, just 23 people — about 32 percent — saw their tumors shrink or disappear completely. “We’d love that to be 99 or 100 percent,” says Allison Betof Warner, an oncologist at Stanford University School of Medicine who wasn’t involved with the trial. But, she says, the results are among the best researchers have seen for melanoma that has continued to advance even after treatment with immunotherapy drugs.
What stands out to Brian Gastman, the executive vice president of medical affairs at Iovance, is how long patients who do well on the treatment can stay healthy — in some cases, years.
In a longer-term analysis of a larger group of trial participants, 48 of 153 people responded to Amtagvi and nearly half of them were still alive at the study’s four-year follow-up, researchers reported in 2023 at the ESMO Immuno-Oncology Congress.
“We know that people are alive today because of this drug,” Gastman says. Scientists still can’t predict the end point of Amtagvi’s tumor-fighting effects, he says. “We haven’t even gotten there yet. We have no idea.”
After Amtagvi’s approval in February, cancer centers around the country began preparing to offer patients the drug. As of May, Iovance reported that more than 100 patients had enrolled for Amtagvi therapy. The company has also taken steps to gain approval elsewhere, including in the European Union, the United Kingdom, Canada and Australia.
Scientists are also trying to make Amtagvi work in a larger proportion of advanced melanoma patients. An ongoing clinical trial, for example, is combining the therapy with checkpoint inhibitor drugs. Early results suggest this combo can increase the number of people who benefit from TIL. Of 22 metastatic melanoma patients who received the combo treatment, nearly 64 percent showed some response, researchers reported in May at the annual meeting of the American Society of Clinical Oncology.
“It’s a very exciting time to be in the field,” Poch says.
As for Rosenberg, who has been at the forefront of cell therapy research for decades, finally seeing FDA approval for a TIL therapy felt gratifying, he says. Still, Amtagvi’s high price tag — $515,000 per patient — is one barrier to widespread availability, Rosenberg wrote in a recent editorial in Science. And he still thinks about the people for whom TIL doesn’t work. You go into one patient’s room and they’re responding to treatment, Rosenberg says, but in the next room over, there’s a patient who’s not.
“It’s a roller coaster,” he says. His team and others are working to figure it out — and how to tailor TILs to other solid tumors. “That’s 100 percent of what we’re doing now,” he says.
English’s last scan was August 2, and she’s still cancer-free more than six years after receiving her TILs. Her next scan is in February. “Hopefully I’m still going to be negative for a long, long time,” she says.
In the time since her treatment, English has picked up a new passion: supporting others with mucosal melanoma. She helped build a website about the disease, coaches people who’ve been newly diagnosed and facilitates weekly Zoom calls for patients and caregivers where she shares her treatment experiences.
“Being able to share that and motivate and help other people on their journey,” she says, “is why I get up every day.”




