"Could This Advanced MRI Reveal Hidden Issues in Your Concussion?"
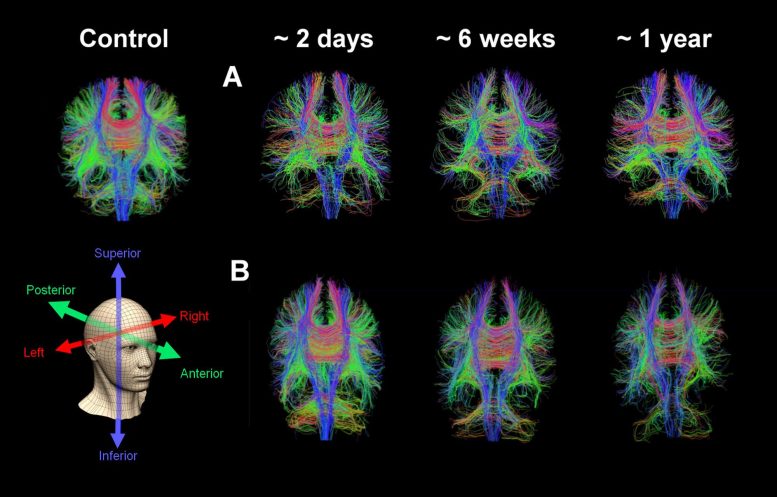
Whole brain diffusion tensor tractography in an age-matched control subject and two patients with serial images at approximately two days, six weeks, and one year following severe traumatic brain injury. Credit: Virginia Newcombe/University of Cambridge
Researchers in Cambridge suggest that diffusion tensor imaging (DTI), a specialized MRI, could significantly improve concussion diagnosis by identifying patients at risk of long-term symptoms, which often go undetected with traditional CT scans.
The study showed that DTI, along with certain blood biomarkers, could predict with much higher accuracy which patients would have persistent symptoms, thus potentially transforming how concussions are managed in clinical settings.
Offering patients with concussion a type of brain scan known as diffusion tensor imaging MRI could help identify the one in three people who will experience persistent symptoms that can be life-changing, say Cambridge researchers.
Around one in 200 people in Europe every year will suffer concussion. In the UK, more than 1 million people attend Emergency Departments annually with a recent head injury. It is the most common form of brain injury worldwide.
When a patient in the UK presents at an Emergency Department with head injury, they are assessed according to the NICE head injury guidelines. Depending on their symptoms, they may be referred for a CT scan, which looks for brain injuries including bruising, bleeding, and swelling.
However, CT scans identify abnormalities in fewer than one in 10 patients with concussion, yet 30-40% of patients discharged from the Emergency Department following a scan experience significant symptoms that can last for years and be potentially life-changing. These include severe fatigue, poor memory, headaches, and mental health issues (including anxiety, depression, and post-traumatic stress).
Dr. Virginia Newcombe from the Department of Medicine at the University of Cambridge and an Intensive Care Medicine and Emergency Physician at Addenbrooke’s Hospital, Cambridge, said: “The majority of head injury patients are sent home with a piece of paper telling them the symptoms of post-concussion to look out for and are told to seek help from their GP if their symptoms worsen.
“The problem is that the nature of concussion means patients and their GPs often don’t recognize that their symptoms are serious enough to need follow-up. Patients describe it as a ‘hidden disease’, unlike, say, breaking a bone. Without objective evidence of a brain injury, such as a scan, these patients often feel that their symptoms are dismissed or ignored when they seek help.”
In a study published today (August 8) in the medical journal eClinicalMedicine, Dr. Newcombe and colleagues show that an advanced form of MRI known as diffusion tensor imaging (DTI) can substantially improve existing prognostic models for patients with concussion who have been given a normal CT brain.
DTI measures how water molecules move in tissue, providing detailed images of the pathways, known as white matter tracts, that connect different parts of the brain. Standard MRI scanners can be adapted to measure this data, which can be used to calculate a DTI ‘score’ based on the number of different brain regions with abnormalities.
Dr. Newcombe and colleagues studied data from more than 1,000 patients recruited to the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study between December 2014 and December 2017. 38% of the patients had an incomplete recovery, meaning that three months after discharge their symptoms were still persisting.
The team assigned DTI scores to the 153 patients who had received a DTI scan. This significantly improved the accuracy of the prognosis – whereas the current clinical model would correctly predict in 69 cases out of 100 that a patient would have a poorer outcome, DTI increased this to 82 cases out of 100.
The researchers also looked at blood biomarkers – proteins released into the blood as a result of head injury – to see whether any of these could improve the accuracy of the prognosis. Although the biomarkers alone were not sufficient, concentrations of two particular proteins – glial fibrillary acidic protein (GFAP) within the first 12 hours and neurofilament light (NFL) between 12 and 24 hours following injury – were useful in identifying those patients who might benefit from a DTI scan.
Dr. Newcombe said: “Concussion is the number one neurological condition to affect adults, but health services don’t have the resources to routinely bring back every patient for a follow-up, which is why we need a way of identifying those patients at greatest risk of persistent symptoms.
Current methods for assessing an individual’s outlook following head injury are not good enough, but using DTI – which, in theory, should be possible for any centre with an MRI scanner – can help us make much more accurate assessments. Given that symptoms of concussion can have a significant impact on an individual’s life, this is urgently needed.
The team plan to look in greater details at blood biomarkers, to see if they can identify new ways to provide even simpler, more practical predictors. They will also be exploring ways to bring DTI into clinical practice.
Dr. Sophie Richter, a NIHR Clinical Lecturer in Emergency Medicine and first author, Cambridge, added: “We want to see if there is a way to integrate the different types of information obtained when a patient presents at hospital with brain injury – symptoms assessment, blood tests and brain scans, for example – to improve our assessment of a patient’s injury and prognosis.”
The research was funded by European Union’s Seventh Framework Programme, Wellcome and the National Institute for Health and Care Excellence.
Reference: “Predicting recovery in patients with mild traumatic brain injury and a normal CT using serum biomarkers and diffusion tensor imaging (CENTER-TBI): an observational cohort study” 8 August 2024, EClinicalMedicine. DOI: 10.1016/j.eclinm.2024.102751




