FDA to Ban Ineffective Cold Medicine Ingredient—Impact on Consumers
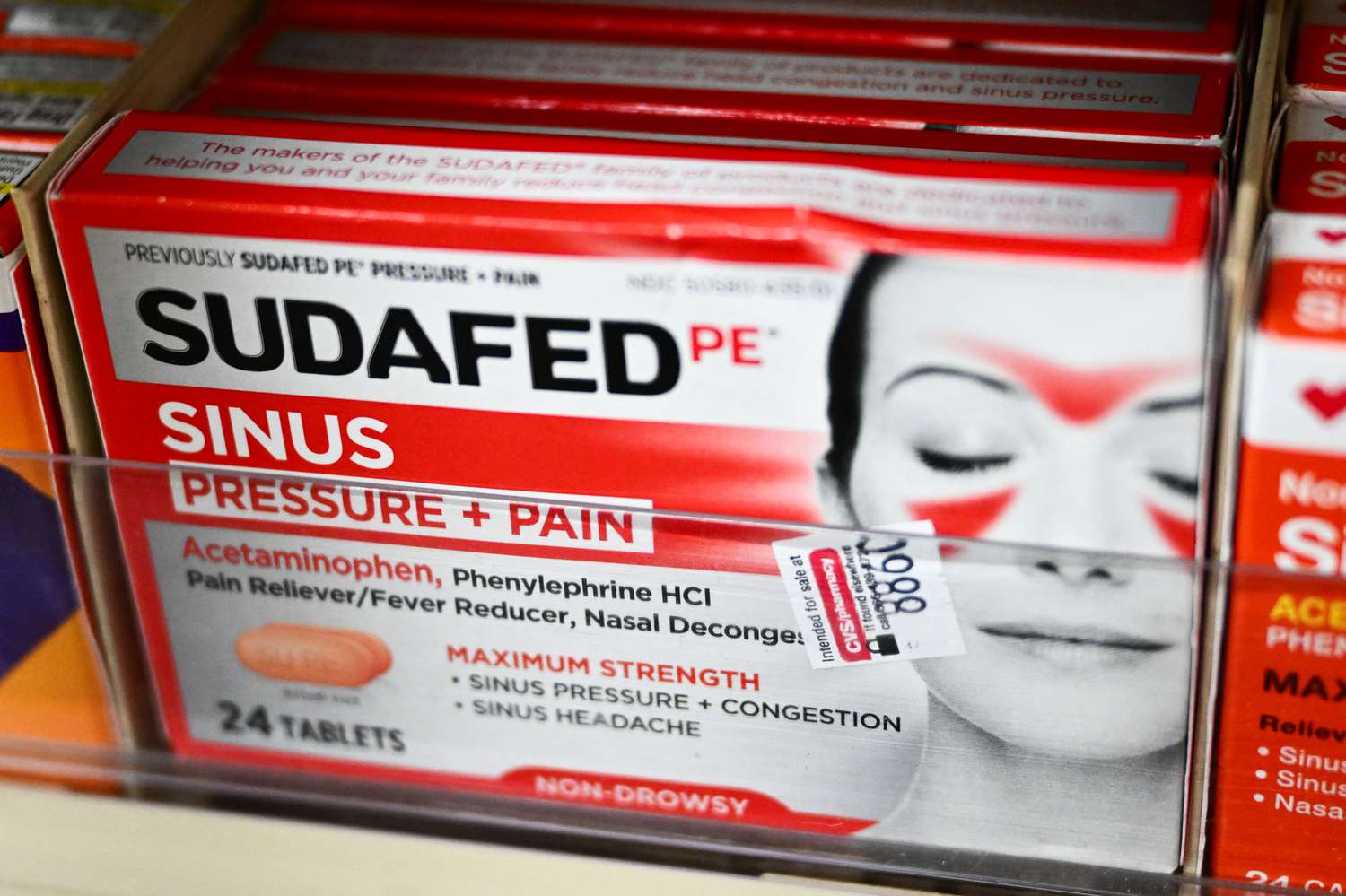
Phenylephrine, a common ingredient in over-the-counter cold medications like DayQuil, Theraflu, and Sudafed, may soon be banned from drugstore shelves.
On Thursday, the Food and Drug Administration announced its proposal to remove phenylephrine from the approved listed of over-the-counter drugs to treat nasal congestion, citing evidence that the oral version of the medication is ineffective. This proposal comes about a year after an FDA advisory committee concluded that the drug doesn’t work.
The proposal is open for public comment until May 7, 2025—after which the FDA will make its final decision. Until then, companies can continue to make and market oral phenylephrine for nasal congestion, as the proposal is based on the drug’s effectiveness, not on safety concerns.
The FDA’s proposal only applies to orally administered phenylephrine, like in tablets or capsules, and not the nasal spray form.
“It is the FDA’s role to ensure that drugs are safe and effective,” Patrizia Cavazzoni, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a statement. “Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant.”
Phenylephrine is widely used in cold and allergy medication to treat nasal congestion, as it’s thought to work by reducing swelling of the blood vessels in the nasal passages.
Phenylephrine isn’t always listed on the front of the box, as these products tend to contain multiple ingredients to treat various symptoms, so it’s best to check the active ingredients on the product label.
Brand names of oral phenylephrine products include:
There are even more combination products of oral phenylephrine plus other drugs. The National Library of Medicine has a full list of medications that include phenylephrine as an active ingredient; some of the most common brands are:
Phenylephrine became a popular ingredient in over-the-counter cold medicine in 2006, when the Combat Methamphetamine Epidemic Act was signed into law.
Before then, an effective oral decongestant called pseudoephedrine was the go-to ingredient in these medications. But the law banned over-the-counter sales of cold medicines that contained pseudoephedrine—including the brand name Sudafed—because it was commonly used to make methamphetamine.
Leslie Hendeles, PharmD, professor emeritus at the University of Florida College of Pharmacy, told Health that “phenylephrine can’t be made into methamphetamine, and drug companies, not wanting to lose the market, immediately switched to phenylephrine,” which the FDA deemed safe and effective for treating nasal congestion in the 1970s.
However, in 2007, Hendeles and his colleagues published a paper with research that oral phenylephrine did not treat nasal congestion any more than placebos did. “It turns out, if you go back and analyze the studies that were used, the panel reached a specious conclusion, and the old data does not show that it’s effective either,” Hendeles said.
At the time, the FDA used other research to conclude that oral phenylephrine could still work, but around 2015, several more studies came out that showed the drug was ineffective. These studies had stronger designs than the previous research, with large sample sizes and double-blind methods.
Based on the strength of this new data, in September 2023, the FDA advisory committee concluded that oral phenylephrine did not work in treating nasal congestion.
There are still a wide variety of over-the-counter medications available to treat nasal congestion related to allergies or the common cold. “The FDA removing phenylephrine is not going to deprive any patients,” Hendeles said.
For patients with a common cold, Hendeles recommends nasal spray with phenylephrine. He explained that when phenylephrine is activated in the gut after being swallowed, it doesn’t get effectively absorbed into the blood stream. When the same drug is sprayed into the nose, it can relieve nasal congestion.Henedeles also recommend oral pseudoephedrine, which is still available for adults age 18 or older without a prescription behind the pharmacy counter.
Sterling Elliott, PharmD, a clinical pharmacist and assistant professor of orthopedic surgery at the Northwestern University Feinberg School of Medicine, also recommended oral pseudoephedrine. “To this day, the tried and true oral option remains pseudoephedrine. You can buy it—you simply have to buy it under the controlled conditions,” he told Health. “But it still works great.”
Both Elliot and Hendeles warned against overusing nasal sprays. Using a nasal decongestant daily for more than a week can lead to congestion rebound, causing blood vessels to swell and making the nose feel even more congested, according to Hendeles.
For individuals with allergies, Hendeles suggested two main categories of safe and effective products: nasal steroids such as Flonase, and antihistamine nasal sprays like Astepro.
Elliot mentioned that the proposal is still pending finalization. If you currently use a medication containing oral phenylephrine that works well for you, there is no need to discontinue use. However, if you are thinking about changing your medication, the FDA advises consulting your healthcare provider or pharmacist for other safe and effective alternatives to address your symptoms.




