Promising Gene Editing Technique for Reducing LDL Cholesterol Levels
In Philadelphia, ten critically ill patients participated in a trial for an experimental medication. They all had a genetic cholesterol disorder, heterozygous familial hypercholesterolemia, that increases the level of LDL or “bad cholesterol” in their blood, placing them at high risk of early severe heart disease and premature mortality.
This genetic disorder increases LDL cholesterol in the blood since birth and for some patients, conventional cholesterol-cutting medications failed to control it satisfactorily reveals Andrew Bellinger, the chief scientific officer at Verve Therapeutics and a practicing cardiologist. Verve Therapeutics is a biotechnology firm located in Boston.
VERVE-101, a new form of genetic medicine designed to deactivate a cholesterol-enhancing gene, was then tried out by Bellinger's team. This new therapy employs a unique molecular tool to erase a DNA letter in order to deactivate the gene. This single genetic change can offer a potential lifelong treatment using just one medication.
During the American Heart Association meeting in November, Bellinger presented the results of a limited clinical trial called Heart-1, where VERVE-101 successfully reduced LDL cholesterol levels. This was the first-ever demonstration that a DNA letter change inside a human body could have such effect. “With just one dosage, we can achieve clinically meaningful LDL reductions,” Bellinger stated.
According to Pam Taub, a University of California, San Diego cardiologist who wasn’t part of the trial, familial hypercholesterolemia patients have lifelong symptoms, hence a “one and done” treatment like VERVE-101 can potentially revolutionize treatment strategies for these patients who currently rely on lifelong medication.
Taub expressed concerns about the safety of VERVE-101, citing incidents where a patient suffered a heart attack and another died of cardiac arrest during the trial although Bellinger reiterated that the death was unrelated to the treatment.
Renowned cardiologist Karol Watson from the David Geffen School of Medicine at UCLA welcomed the new revolutionary strategy of editing human DNA to manage cholesterol levels. He underlined the importance of establishing the safety of VERVE-101 while cautioning, “You are changing the genome forever.”
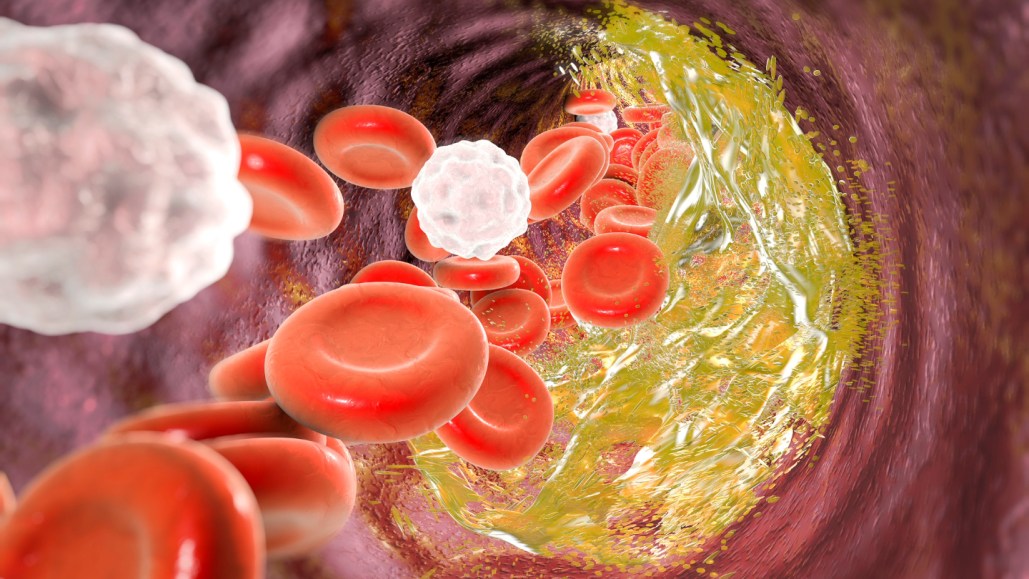
The concoction of VERVE-101 involves two types of RNA molecules contained inside a fat bubble. The drug, which is delivered via infusion, travels to the liver, slipping into cells. While one RNA molecule instructs cells to generate a protein known as an adenine base editor, the other functions as a genetic GPS, leading the editor protein to the correct DNA stretch.
The underpinning of the therapy is CRISPR 2.0 technology. The first generation of CRISPR/Cas9 tools, behaving like molecular scissors can disrupt genes by snipping DNA’s strands. In contrast, base editors act like molecular pencils, rewriting a DNA letter for another and creating a fresh genetic sequence.
"Base editors can actually substitute a chosen sequence into another sequence according to your choice," mentions Howard Hughes Medical Institute investigator David Liu, the chemist at Harvard University whose team invented this technique in 2016. For VERVE-101, the PCSK9 gene which gives instructions for creating a cholesterol-boosting protein is the target. PCSK9 is deactivated with just a single precise location edit.
According to Bellinger, once the infusion is done, the editing process is done within a week and the medication breaks down quickly thereafter. Both the lipid nanoparticle (fat bubble) and its RNA content degrade and in a few weeks, VERVE-101 is completely cleared from the body. While the only evidence of its action is the alteration made to the PCSK9 gene.
PCSK9 has been a major therapeutic target for about the past decade, according to Parag Joshi, a preventative cardiologist at UT Southwestern Medical Center in Dallas who wasn't part of the trial. Joshi notes that some people with PCSK9 mutations tend to have lower LDL cholesterol levels and significantly less heart disease instances as reported by Helen Hobbs, a geneticist and HHMI investigator at UT Southwestern Medical Center, and colleagues in 2006.
The groundbreaking research significantly moved the field forward, highlights Joshi. It was a revelation to scientists when the evidence showed that people could lead healthy lives with inactive PCSK9. This revelation made PCSK9 a promising drug target; Joshi explains that it indicated that incapacitating PCSK9 could potentially reduce the risk of heart disease without causing harm.
Normally, the PCSK9 protein deactivates another protein called the LDL receptor. This receptor acts as a regulator of bad cholesterol by transporting it into liver cells for elimination, therefore keeping cholesterol levels under control. But without sufficient LDL receptors, LDL cholesterol levels in the blood increase aggressively.
Verve's CEO and cardiologist Sekar Kathiresan puts it simply that PCSK9 causes disease. He further explains that turning off PCSK9 will lead to overall health.
According to Joshi, some current treatments target PCSK9, including therapies using injected antibodies or an RNA-based drug that halts the production of the protein. Patients are generally advised to take a daily statin pill to help reduce LDL cholesterol. However, this often proves insufficient.
While these therapies are theoretically helpful for individuals with familial hypercholesterolemia, Kathiresan points out that a small number of patients are actually using these treatments. He believes this is because the current approach is too demanding— requiring patients to take daily pills or receive periodic injections for many years. "This model doesn't seem to be working," Kathiresan reveals, expressing his team's intention to remedy this issue.
The team headed by Kathiresan administered a single IV infusion of VERVE-101 to 10 individuals with heterozygous familial hypercholesterolemia—most of them suffering from severe heart disease. In those administered with the highest drug dosages tested, a marked drop of 39 to 55 percent in the blood levels of LDL cholesterol was observed. This decrease appears to be enduring. For the patient who received the highest dose, LDL cholesterol levels remained steady for 180 days post the infusion.
Bellinger describes the results as more or less anticipated and planned, considering the previous results from the team's study on nonhuman primates. With the new preliminary patient data, Kathiresan hopes that the drug could offer a revolutionary method to treat heart disease.
The ultimate effectiveness of VERVE-101 will depend on its safety. During the trial, the team noted some possible concerns. Four patients had minor reactions to the IV infusion, such as a mild fever and headache. Later, major incidents caused alarm— one patient suffered a heart attack a day after the infusion, while another died about five weeks post the infusion when their heart suddenly stopped beating.
Kathiresan believes the latter incident was likely due to the patients' existing heart conditions. He adds that this conclusion was backed by an independent data safety monitoring board that reviewed the cases. However, they determined that the heart attack might be linked to the treatment, given the proximity to the timing of the dosage.
Taub, a UCSD cardiologist, highlights that these patients were extremely unwell, suggesting the exclusion of such patients from future trials with the drug. Kathiresan's team now plans to include only patients with less advanced disease and also intend to examine possible blockages in patients' arteries to prevent enrolling patients at extreme risk of heart attack.
Kathiresan reaffirms that the drug could offer a revolutionary way to treat heart disease.
In 2024, the company plans to include more patients at the two highest dosages to finalize the dosage to proceed with. The researchers are also working on a second version of the drug, VERVE-102, which features a different lipid nanoparticle. Keeping the outcome of this in mind, Verve intends to advance one of the drugs to a larger clinical trial in 2025. If successful with patients with familial hypercholesterolemia, the company aims to widen the pool of patients to include individuals who do not have the genetic disorder.
Kathiresan reminds everyone that the process of developing new drugs is lengthy, with drugs typically taking over a decade to transition from an idea to a prescribable medication. Verve began its project on PCSK9 editing in 2018. By the end of the decade, Kathiresan hopes to have an approved drug.
One potential side effect of gene-editing therapies is unintentional tweaks to DNA. VERVE-101 targets PCSK9, but what if it strays to a different spot in the genome, asks Anne Goldberg, an endocrinologist at Washington University School of Medicine in St. Louis. The technology “looks really interesting,” she says, “but we need more data.”
A DNA change at the wrong spot could put people at risk of developing cancer. With VERVE-101, Bellinger said, “we think that risk is very low.” Most of the company’s work, he said, goes into demonstrating that “we do not make edits elsewhere in the genome.”
Today’s base editors — including the one in VERVE-101 — are much improved since the early days of the technology, says Harvard’s Liu, who was not involved with the trial. They “have very high on-target editing efficiency while also having minimal off-target editing.”
Currently, five other base-editing clinical trials targeting other diseases, like sickle-cell disease and leukemia, are ongoing. Liu is hopeful that the gene-editing agents will give patients “a completely new lease on life.”
Bellinger said his team thinks of VERVE-101 as a one-time procedure for health, like “molecular surgery without a scalpel.” In theory, it’s possible to reverse the edit made by VERVE-101, but it’s not what he and his colleagues envision.
For cardiologist Donald Lloyd-Jones, who was not involved with the trial, the dream is to offer people with familial hypercholesterolemia a treatment that doesn’t rely on taking a statin pill every single day. A therapy like VERVE-101 “might be something they really consider as an option,” said Lloyd-Jones, of Northwestern University Feinberg School of Medicine in Chicago.
“If we get those safety data, if we get those efficacy data,” he said at the meeting, “I think this would be a very interesting approach to a lifetime fix.”




